Prior Authorization Today is Challenging – MRIoA Makes it Easy
Reimagine Prior Authorization Flow with ClearPath PriorAuth™ by MRIoA
Prior authorization has never been tougher. Patients wait for answers and struggle to make treatment decisions with confidence within a system that does not offer treatment alternatives easily.
Providers grapple with what treatment needs a PA, and what does not, in a healthcare landscape where PA systems do not clearly outline recommendations or tie directly to EMRs.
Payers strive to maintain cost controls while ensuring appropriate care, but high clinical variation; administrative hurdles, and conflicting information create confusion and complexity.
With MRIoA, you can transcend the noise, speed the PA process and walk “a clear path to clinically relevant simplicity.”

End to End PA Triage
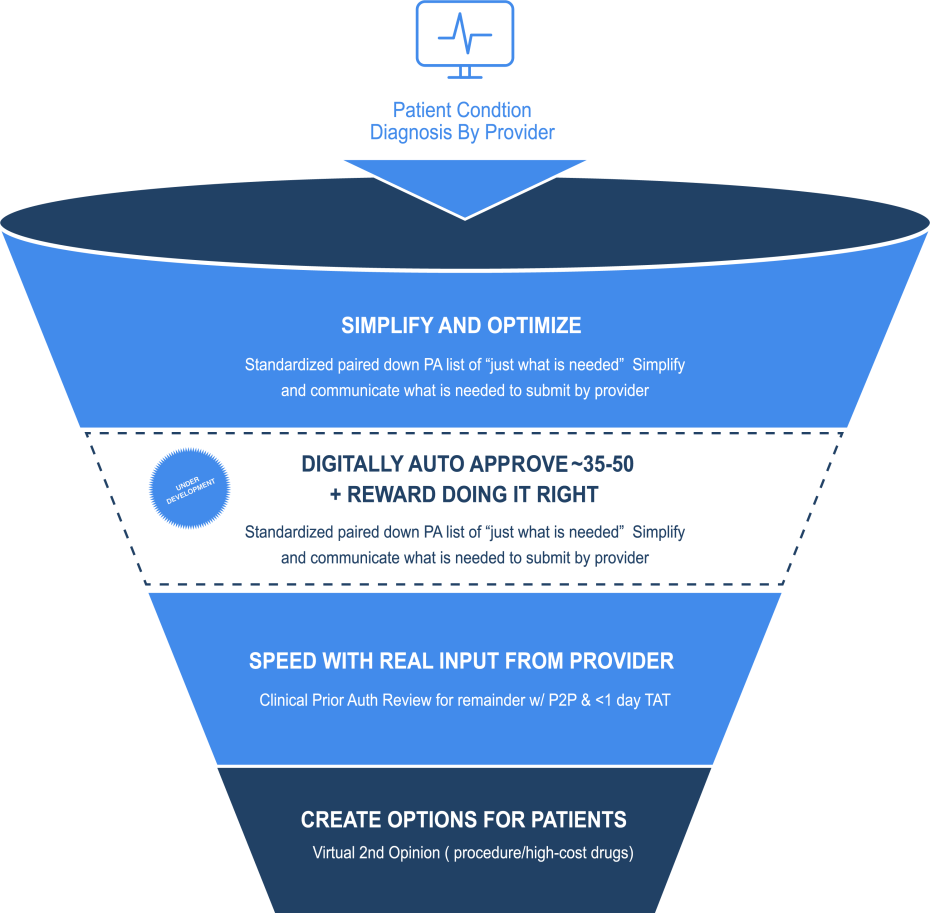
PRIOR AUTHORIZATION OPTIMIZATION
Our Prior Authorization optimization services give you confidence to prior authorize what you need – and stop wasting time on what you don’t. PA Optimization™ is the simple way to enable the right care, at the right time, in the right place while reducing friction for patients, providers and payers. By partnering with MRIoA, our clients can reduce unnecessary care by $10M over a three year period per 100K members with a 7:1 ROI.
PROACTIVE TELEHEALTH SECOND OPINIONS
MyCareChoices™ delivers a telehealth 2nd opinion from a MD specialist as part of the approved Prior Authorization process. This enables the member to better understand their condition and treatment options so they can make the best decision for themselves and their family. MyCareChoices™ delivers ~$800K per 100K members in savings by reducing unneeded procedures and requires no IT integration.
OPTIMIZE HIGH-COST SPECIALTY DRUG SPEND
MRIoA’s specialty drug reviews allow health plans, TPAs and PBMs to leverage MD specialists to ensure adherence to evidence-based guidelines for high-cost drugs. Supporting the treatment for medical conditions where a therapeutic interchange is available to maintain the same efficacy for the patient while reducing cost.
PROVIDER GOLD CARD SERVICES™
Gold carding physicians involve granting certain providers the ability to bypass or streamline the prior authorization process based on their history of high-quality care and adherence to evidence-based guidelines. MRIoA’s solution eases the strain on internal staff, reduces cost, ensures the right care and helps you stay compliant.
By combining all of these elements into a customized solution for your health plan or TPA, we deliver significant savings, significant clinical value, a simpler process for providers leading to options and education for the patients you serve.

Our MRIoA ClearPath solution streamlines the prior authorization process by delivering targeted utilization management and patient transparency so you can operate efficiently, increase clinical value, and save on administration costs.
The benefits of ClearPath include:
-
Streamlined workflow
-
Faster authorization turnaround time
-
Cost reduction
-
Improved patient access to care
-
Increased provider productivity
-
Reduced provider-payer communication
PA Optimization
MyCareChoices™
Patient Education
High-cost Specialty Drug Review
Provider Gold Card Services
Resources
Drive Cost Savings and Elevate Patient Care
Experience valuable data insights, cost savings, and faster decision-making with our innovative technology and patient-centered approach.
A ClearPath to Clinically Relevant Simplicity.
Meet with one of our experts to get started.