Prior Authorization Optimization Solutions from MRIoA Deliver Both
Let’s Streamline Your Prior Authorization
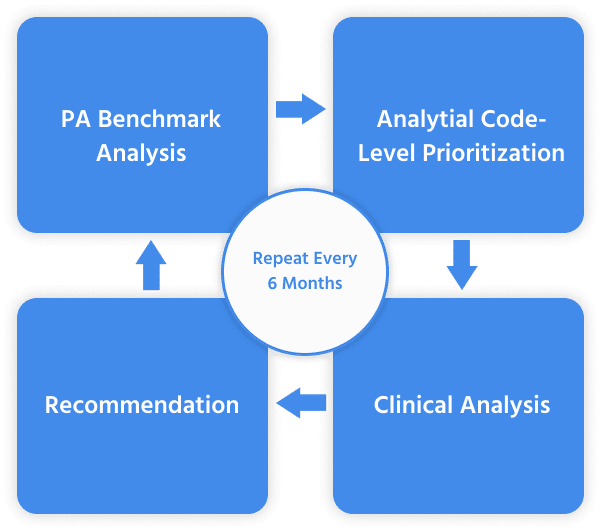
Over and underutilization resulting from sub-optimized PA list, or not having the capacity to administer the program, can lead to member frustration as well as higher aggregate service costs. Our reviews efficiently identify areas of savings and improvement and also help you eliminate what is not needed. Every 6 months, MRIoA’s PA Optimization™ analytics team performs a customized CPT code-level ROI assessment that enables health plans to manage a more targeted prior authorization list.
With MRIoA’s Prior Authorization optimization services, payers can confidently prior authorize only what is needed and reduce the administrative burden of unnecessary prior authorizations. Our clients reduce unnecessary care by $10M over a three year period per 100K members delivering the “right care, at the right time, in the right place.”
At MRIoA, we believe PA should be more focused and less burdensome. Reducing the services that require PA based on data analytics does just that!
Recurring Analytic Processs
Savings Off of Year Zero Baseline:

Total 3-Year Savings: $10M
PA Optimization Program Analysis Typical Plan 100K Commercial Members
$1.7M Savings Annually
7:1 ROI
Per 100K Lives
Manage Prior Authorizations to Improve Outcomes and Reduce Costs
MRIoA’s PA Optimization platform enables health plans to design and manage a better prior authorization solution, with better quality and reduced provider abrasion.
UM Market Benchmarks
MRIoA PA Optimization consolidates industry-wide UM research and CPT code-level ROI analytics to help Health Plans create a targeted prior authorization list.
UM Performance Analytics
MRIoA PA Optimization provides up-to-date benchmarking at the procedure level to ensure the best real-time UM program decisions.
Clinical Utilization Review
MRIoA provides flexible clinical review solutions to realize immediate benefit from the PA Optimization recommendations.
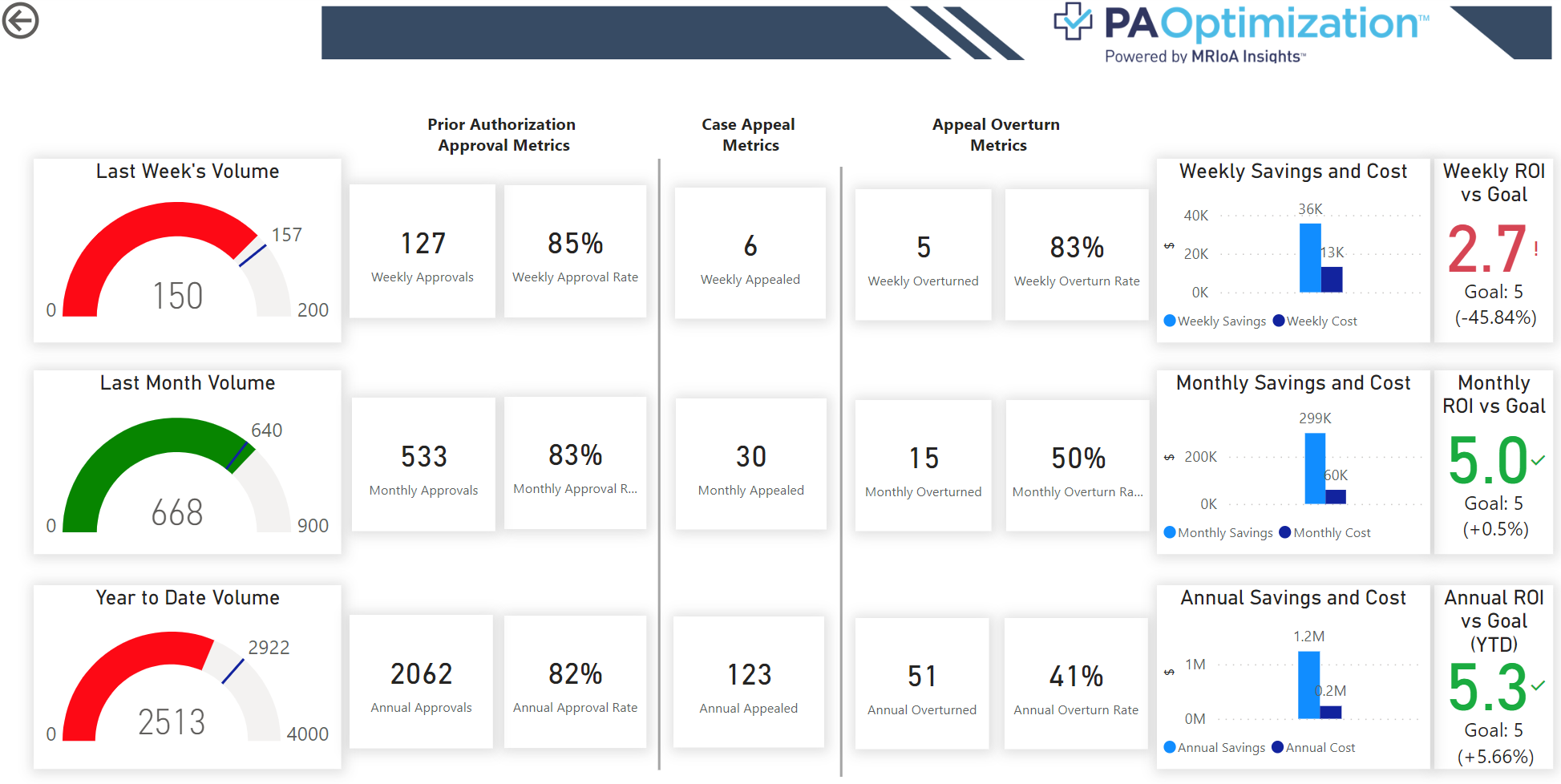
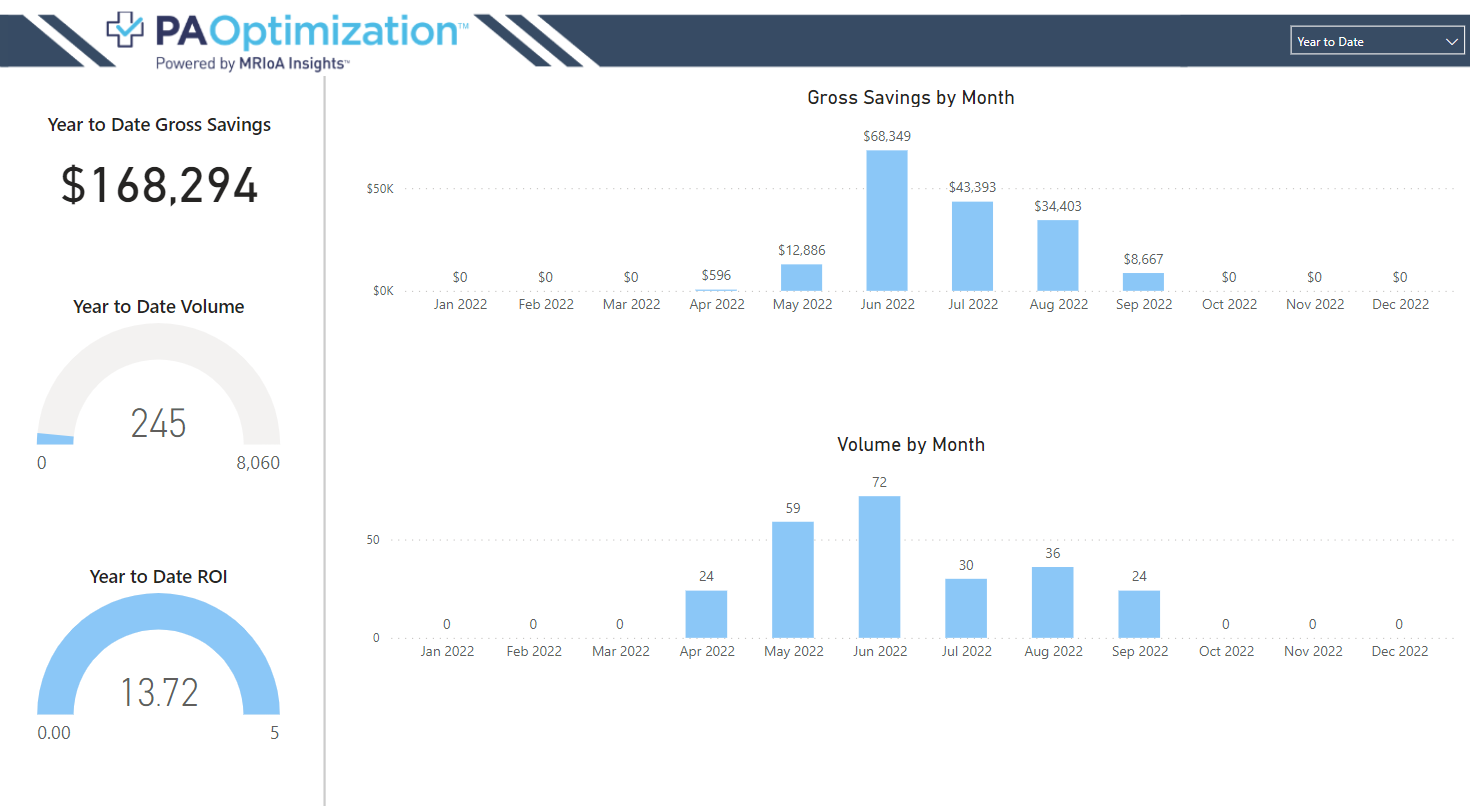
PA Optimization Reports Powered by MRIoA Insights™
Gain valuable insights as to what to prior authorize and what to eliminate. These reports help to reduce patient, provider and payer burden on what to prior authorize.
Resources
Drive Cost Savings and Elevate Patient Care
Experience valuable data insights, cost savings, and faster decision-making with our innovative technology and patient-centered approach.
A ClearPath to Clinically Relevant Simplicity.
Meet with one of our experts to get started.